


Morten’s neuroma Vs plantar plate

Morten’s neuroma Vs plantar plate
If you’ve ever suffered from pain in the ball of your foot you’ll know only too well how annoying and debilitating it can be. However, addressing the cause of the pain starts with the right diagnosis.
Two widespread causes of forefoot pain are Morten’s neuroma and plantar plate trauma. While plantar plate tears are less well known and identified, they are clinically prolific.
Morten’s neuroma
A Morten’s neuroma is a nerve injury. The joints around the metatarsal bones rub together causing irritation and swelling, which encroaches on the nerves. The nerves can become damaged and thickened resulting in the shooting, stabbing pain and burning sensation linked with a Morten’s neuroma.
The nerves in the intermetatarsal spaces (between the 2nd-3rd and 3rd-4th toes) are most commonly affected leading to pain in the ball of the foot.
Symptoms of Morten’s neuroma
- A sharp, shooting pain in the ball of the foot (usually between third and fourth toe)
- A burning pain in the ball of the foot that may spread or shoot down towards the toes
- Toes may feel numb or tingle
- Pain is intensified when wearing tight shoes or high heels

Podiatrist and founder of A Step Ahead Foot + Ankle Care Dr Brenden Brown explains, “Wearing high heels or tight fashion shoes compresses the nerve and creates that electric, shooting pain.
“People with foot deformities, such as hammertoes, bunions, flat feet or high arches, are at higher risk of a Morten’s neuroma because these defects generally cause the foot to widen, making it more difficult to find shoes that aren’t tight.”
Treatment for a Morten’s neuroma
Treatment will depend on the severity of symptoms but first-line treatment options include:
- Appropriate footwear—avoid shoes that are narrow in the forefoot or tight in general
- Soft tissue rehabilitation — Soft tissue massage to the Morten’s region can provide some relief from the associated pain
- Soft cushioned orthotics with a metatarsal dome may help reduce pressure on the nerve
- Injections to reduce inflammation, such as cortisone or Prolotherapy
- Surgical opinion is required if conservative measures are unsuccessful

Plantar plate tear
This is the very start of clawed or hammer toes! A plantar plate injury involves the ligament and cartilage attached to the base of and between our toe bones (phalanges). Injury can involve tears, ruptures or distensions. Conservative treatment for this condition is highly effective.
Symptoms of plantar plate tear
- Dull ache or sharp pain under the ball of the foot
- A “V” sign where the toes separate and form a V shape
- Toe lifts upwards (commonly the 2nd or 3rd toe) and may become swollen
- In acute cases the toe becomes thickened or enlarged. Often described as “sausage like”
- Feeling that you have a small stone in your shoe when walking
- The feeling that there’s insufficient cushioning between the toe bones and the ground
- Small amount of callous develops under the metatarsal heads
- Surgical opinion is required if conservative measures are unsuccessful
Treatment for plantar plate tear
- Conservative treatment for this condition is highly effective if caught within the first 6 – 12 months
- Wearing firm, stiff-soled shoe can help alleviate pressure on the joint and reduce the pain
- Cushioned orthotics with a metatarsal dome (often recommended by orthopaedic surgeons)
- Soft tissue rehabilitation, deep connective tissue therapies to the joint capsules and the spaces around this area.
- Deep connective tissue therapies to the extensor and flexor tendons and muscles of the foot
- Serial strapping or taping to prevent the toes popping up or hold them in alignment
Dr Brenden says, “For years Morten’s neuroma has widely been the most common diagnosis for forefoot pain. Yet I find that in many cases, where there is a dull ache type of pain in the ball of the foot, the cause is a plantar plate tear rather than Morten’s neuroma.”
Radiology
Morten’s neuroma and plantar plate trauma are difficult to distinguish between on diagnostic ultrasound.
“When viewed in ultrasound the two conditions without further discovery and without an experienced radiologist can appear the same. The two conditions will often return a hypoechoic mass finding, hence the need for more detailed clinical symptoms and signs accompanying the request.
“Given that the difference in symptomatology between the two is often the key, clinical symptomatology should be included in the radiological request,” advises Dr Brenden.
Related articles
4 hacks to staying injury free this winter sports season
5 hacks to keep ingrown toenails at bay
Your guide to sock solid ankle stability
About us
A Step Ahead Foot + Ankle Care is one of Sydney’s leading foot and ankle clinics. Principal podiatrist and founder of A Step Ahead Dr Brenden Brown (AKA Dr Foot) has been taking care of people’s feet for more than 20 years.
With a background in sports medicine and having served as a former president of the Australasian Podiatry Council, Brenden is a wealth of information when it comes to foot and ankle care.

Ingrown toenail surgery—is it right for you?

Ingrown toenail surgery—is it right for you?
What does ingrown toenail surgery involve?
Surgery to address an ingrown toenail (onychocryptosis) involves removing the bothersome nail and applying a chemical to prevent the nail from growing back.
In some instances it may be necessary or most beneficial to remove a small section of nail at one or both sides, but on the odd occasion the entire nail (total nail avulsion) will be removed.
It is a quick and simple procedure than is essentially pain free as it is performed with an injection of local anaesthetic.
Following surgery the toe is dressed and generally speaking there is little, if any, pain or discomfort. You may expect some throbbing that night or discomfort but this is most often managed well with paracetamol.
When is toenail surgery the best option?
Ingrown toenail surgery should not be considered first-line treatment for an ingrown toenail. It can be considered when:
- Other non-surgical methods have been exhausted
- The nail is involuted or curved
- Ingrown toenail is problematic, painful or recurring
- You understand the implications and potential complication of surgery
- You have discussed any concerns with your podiatrist
What are the advantages of clinic-based toenail surgery?
- No time in hospital
- No Sutures / stitches required – all completed under the nail plate
- No more recurrent ingrown toenails
- Pain free
- Minimal time off work
- Reduced episodes of infection and lesions (weeping, bleeding)
- In the majority of cases, ingrown toenail surgery is very successful
Dr Brenden Brown, podiatrist and founder of A Step Ahead Foot + Ankle Care, says, “Nail surgeries are not new for podiatrists; we perform them on a regular basis. It is part of our training at University so we are well versed in this surgery. It is carried out in our clinic and, due to our high level of training, is a fairly simple procedure.
“I often describe this surgery as ‘relatively pain free’. It is wrong to say any surgical procedure is ‘completely pain free’ but as procedures go our patients report very little, if any, pain. In fact, patients are frequently surprised at just how pain free it actually is!
“This procedure can certainly be of benefit and is recommended for patients who have a history of infection or recurrent ingrown toenails. It’s also very helpful for patients with involuted or very curved nails and toenails with areas that seem to catch the skin on the side of the nail.
“Patients often suffer from an ingrown toenail for many years with little idea where to go to for help.
“The days of painful surgeries with patients regularly experience nail re-growth are gone. It’s also important to remember that what you see on YouTube and other social media sites is often the ‘most horrible’ and ‘most atrocious’. If it wasn’t so gruesome you probably wouldn’t have been so motivated to watch and it likely would have got the “views” it did!
Related articles:
5 hacks to keep ingrown toenails at bay
ABOUT US
A Step Ahead Foot + Ankle Care is one of Sydney’s leading foot and ankle clinics. Principal podiatrist and founder of A Step Ahead Dr Brenden Brown (AKA Dr Foot) has been taking care of people’s feet for more than 20 years.
With a background in sports medicine and having served as a former president of the Australasian Podiatry Council, Brenden is a wealth of information when it comes to foot and ankle care.
Got a question? Check out our Instagram profile #AskDrFoot
Tune into our Facebook page for regular live videos and updates on the latest foot and ankle advice from the experts.

5 hacks to keep ingrown toenails at bay
5 hacks to keep ingrown toenails at bay
What causes an ingrown toenail?
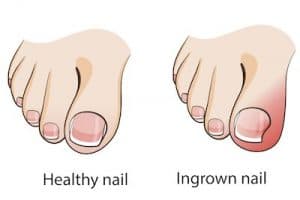
Ingrown toenail (known medically as onychocryptosis) is a condition where the edge of the toenail (most commonly on the big toe) pierces or catches on the skin as it grows up.
MYTH: Nails only grow upwards they do not on any occasion grow outwards towards the side.
There are several causes of an ingrown toenail but probably the most widespread is poor toenail-trimming technique. Cutting down the side of the nail is a major no-no. Why? Because even the smallest spike of nail can grow up and penetrate, or get caught on, the skin.
The ingrown slither of nail acts like a splinter; the skin around it thinks it’s a foreign body and becomes inflamed and infected.

5 hacks to prevent ingrown toenails
- Clip with caution. Trim toenails straight across. DO NOT cut down the sides of the nail and refrain from cutting nails too short
- Refrain from ripping the nails down the sides. We have all done this! You cut but you can’t get that last bit of nail, so you abandon the clippers and rip the last piece down the side. This leaves a sharp spike, which may not be painful now but in following days it will grow upwards and catch on the skin piercing it creating the subsequent infection and PAIN!
- Ditch footwear that is too tight or constricts the toes from moving. This can push the nail into the skin causing irritation and infection
- Steer clear of unqualified people offering to remove ingrown toenails. While this may sound somewhat self-serving, there are an increasing number of nail salons offering to perform this sort of work. Removing the nail breaks the skin barrier, which can easily become infected. Whilst your podiatrist makes it look easy that is because it’s what they have been trained to do and complete on a regular basis.
- Adhere to best-practice foot care by keeping feet clean and dry to avoid weak, splitting nail and fungal infections.
How to fix ingrown toenails — at home
To treat an ingrown toenail at home you can try: Cutting the nails straight across and applying an antibiotic cream to help reduce the risk of infection and subsequent inflammation. You can also use a nail file to round the corners!
MYTH: Cutting a V in your toenail will not make it grow inwards; nails only grow upwards. While the V may look like it’s closing in, this is an illusion as you are trimming the top of the V, making it appear like the V is getting smaller over time.
Applying a small piece of cotton wool between the ingrown nail and the skin can help life the nail, hopefully clearing it and preventing the nail from piercing the skin again.
Avoid wearing high heels, pointed or tight fitting shoes as these can place pressure on the affected area, potentially delaying healing.
The professional approach
Dr Brenden Brown, podiatrist and founder of A Step Ahead Foot + Ankle Care, says, “If the toenail turns into a monster and becomes red, angry or infected—It’s definitely time to seek professional advice.
“A podiatrist can easily treat an ingrown toenail by removing the troublesome spike of nail. In most cases this is a quick (takes minutes) and simple procedure, which is completely painless.
“Following the removal of the nail spile, the toenail area is cleaned and, if infection has been present, the toe will be dressed.
“In extreme cases, toenail surgery may be required. This will generally only happen if the patient has a repeated history of recurrent in grown nails or if the nails shape means it requires removal of that section, such as when it is involuted or excessively curved.
“It is more rare than most people think to remove a whole nail as we can manage these well conservatively”
Related articles:
Ingrown toenail surgery—is it right for you?
ABOUT US
A Step Ahead Foot + Ankle Care is one of Sydney’s leading foot and ankle clinics. Principal podiatrist and founder of A Step Ahead Dr Brenden Brown (AKA Dr Foot) has been taking care of people’s feet for more than 20 years.
With a background in sports medicine and having served as a former president of the Australasian Podiatry Council, Brenden is a wealth of information when it comes to foot and ankle care.
Got a question? Check out our Instagram profile #AskDrFoot
Tune into our Facebook page for regular live videos and updates on the latest foot and ankle advice from the experts.

Taking care of common kids’ foot complaints

Taking care of common kids’ foot complaints
While most parents worry about the health of their child’s eyes and teeth, many overlook the state of their kids’ feet. Feet are amazing; not only do they enable us to stand tall and move, they support our body weight and act as shock absorbers, in turn protecting our ankles, knees, hips and spine.
In young children the foot is pliable to allow it to develop, which means taking care of feet during the first few years of a child’s life is vital.
Recognising common foot complaints can help ensure that action is taken to address the problem and ensure your child’s feet continue to develop in a healthy way.

Ingrown toenails
Ingrown toenails are common with multiple causes. Widespread causes can include clipping the nails too short, cutting or picking at the edges of the nail, trauma to the nail due to kicking sports, excessively sweaty feet and pressure from footwear. All of these events can create a sharp edge on the nail, which can pierce the skin and lead to an ingrown toenail.
The symptoms of an ingrown toenail (onychocrytosis) can include a sore toe, pain at one side of the toenail and, in severe cases, a pus-filled discharge. In most cases it’s usually the big toe that’s affected.
Closed-toe shoes are likely to increase the intensity of the pain and, if left untreated, it’s common for the toenail to become infected making it difficult to walk and particularly painful to play sport.
To treat an ingrown toenail start by soaking the foot daily in warm, salty water, gently patting dry and applying a topical antiseptic. If possible, refrain from wearing enclosed shoes.
If the issue does not resolve within a couple of days it may require treatment by a podiatrist. This is a simple procedure that involves removing the small, sharp portion of nail causing the grief and dressing the nail to protect against infection. It usually takes minutes.
In acute cases nail surgery may be required.

Flat feet
In infants flat feet is common because they have a fat pad under the foot that hides the developing arch. By about the age of eight, the foot arch becomes apparent. Yet some children never develop an arch and this is called ‘flat feet’.
Flat feet or pronated feet (foot and ankle roll inwards) can be hereditary or due to muscle length and tone. In some instances the condition causes no pain or discomfort but in other cases flat feet or over pronated feet can cause pain in multiple areas of the body including the foot itself, shins, knees, lower back and Achilles tendons.
A podiatrist can help treat flat feet using orthotics, which hold the feet in their correct position and help relieve the associated pain. A detailed biomechanical analysis is conducted to diagnose which type of orthotics is best (there are many!).
In addition to orthotics, a podiatrist can advise on other measures that can be taken as part of a multi-pronged treatment plan. This may include stretching, strengthening exercises or deep connective tissue massage. Bare in mind that being overweight or wearing poor footwear can contribute to the symptoms of flat feet.
Plantar warts
Warts can be the bane of a parent’s life because they are so easy to contract, yet notoriously difficult to get rid of.
Often mistaken for corns, plantar warts appear as small (less than 5mm) rough, flat bumps on the bottom of the foot—usually on the underside of the toes, heel or forefoot. Some plantar warts have little black dots in the centre. This is caused by small blood vessels.
Warts are the result of a virus, so they are easily transferred to other children and adults and are particularly common in swimming pools, gyms, communal showers and other places that involve water, warmth and bare feet.
There’s a plethora of treatments for plantar warts but many are lengthy and not always successful. If over-the-counter non-prescription medicines don’t work, you can try a prescription medication such as salicylic acid or cryotherapy, which involves freezing the wart with liquid nitrogen.
Alternatively, your local podiatrist can use laser treatment or a small instrument to remove the wart. To prevent future plantar warts, avoid letting your child go barefoot in high-risk places such as public showers and outdoor swimming pools.
Want to know more about taking care of kids’ feet? Visit: mykidsfootdoctor.com.au.
Got a question? Ask Dr Foot
A Step Ahead Foot + Ankle Care is one of Sydney’s leading foot and ankle clinics. Principal podiatrist and founder of A Step Ahead Dr Brenden Brown (AKA Dr Foot) has been taking care of people’s feet for more than 20 years. With a background in sports medicine and having served as a former president of the Australasian Podiatry Council, Brenden is a wealth of information when it comes to foot and ankle care.
Related blogs:

Should I wear a “Moon Boot” for heel pain?
Is wearing a Moon Boot going to help Heel Pain?

Should I wear a “Moon Boot” for heel pain?
The Answer?
NO, but why? Its best to settle on some understandings from the beginning. It is widely understood that it is “soft tissue and tendons that are what become sore in Heel Pain. The idea that Heel Spurs “cause” pain has been debunked and proven incorrect a number of times!
Over the last few years there has been an evolving understanding around how tendons and soft tissue works. Keep this in the front of your mind – “TENDONS HATE CHANGE”. Stopping all activity if you are currently active is a sure-fire way to ensure that when you return to your activity you will also see the return of your heel pain!
Boots can “Change” tendons – in a negative way!
As we said stopping all activity is not good for us. That same principal exists for those who are using an air cast or moon boots. Completely removing the function of the foot and calf will mean these muscles will most likely fatigue and lose condition. At best, you will need a delicate and dedicated rehab process to get you back to normal function.
This includes “tears” in fascia’s! We have found there is an ever-increasing body of evidence suggesting that many radiologically identified tears maybe completely normal and part of a normal aging process!
Patients often ask us at the clinic about “booting” or casting them after “a friends” practitioner did this with them their “friend”. All the evidence base suggests that this is often the wrong way forward. In good conscience, we can’t do this. It should be recognized this was once accepted practice, we know we did it!
However the evidence base suggests doing this will unload the soft tissue completely and can in itself start another chain of events and problems which you only have to overcome later! So NO BOOT!
If by chance you are reading this and you’ve been prescribed a boot. I’d respectfully ask your practitioner about what the current evidence base says about this method of treatment?

Should I change my activity?
You SHOULD make modification to activity; however, a complete stop will mean you either
A. Need to rebuild your activity over quite an extended time.
or
B. Your heel pain is likely to return!
For the moment STOP Jumping of and onto things. For example, on + off a truck, box jumps at exercise class, skipping or other high intensity impacting the heel and forefoot until we have you back to comfortable. We will then slowly load you back up to these activities. As a guide if it hurts STOP IT!
What do I do instead?
Our strong advice is to look for strong supportive cushioned footwear.
What does this mean? Look for the following in Sneaker style or work boot.
1.Always lace up!
2.Bend only at the toes
3.Shoes should NOT bend in the middle!
4.Should NOT twist or wring out
5.Firm heel counter (back of shoe that hugs the heel)
Wear your lace up shoes – From the moment you wake – till the moment you head to bed! No matter inside or outside! No thongs – NO bare feet! This is a far better way of providing the tendons and other soft tissue structures support without immobilizing the foot and creating more problems.

Need some help?
Our Doctors at A step ahead see between 8 – 12 heel pain patient each every day! Heel pain , sports injuries and musculoskeletal pain in feet + lower legs are our passion. We are often for many people the 2nd, 3rd or even 4th opinion for their heel pain. We are most often the last!
First steps to getting back to pain free?
Give our front desk team a call, they speak to dozens of people a day just like you with problematic heel pain. They will run through with you what you may have tried so far and get a better understanding of your pain. They will then help work out what type of appointment is best to make for you. From here they can reserve your appointment time.
We would LOVE to be able to help you on the way back to becoming Happy Healthy + active.
Our number is 96732987 or 47322007 we look forward to helping you
If you are looking for more information we have a prepared a dedicated page to helping both other practitioners and patients with information on HEEL PAIN. ” Heel Pain Doctor ” has loads of fact and helps busts some of the myths around heel pain.





 Dr Brenden’s White paper report on the “6 Reasons You Won’t Beat Heal Pain” outlines what’s stopping you from beating this and tips on how to stop it in its tracks!
Dr Brenden’s White paper report on the “6 Reasons You Won’t Beat Heal Pain” outlines what’s stopping you from beating this and tips on how to stop it in its tracks!